TONGUE DISEASES
Fatma Ceren1
Taha Emre Köse2
1Recep Tayyip Erdoğan University Faculty of Dentistry, Department of Oral and Maxillofacial Radiology, Rize, Türkiye
2Recep Tayyip Erdoğan University Faculty of Dentistry, Department of Oral and Maxillofacial Radiology, Rize, Türkiye
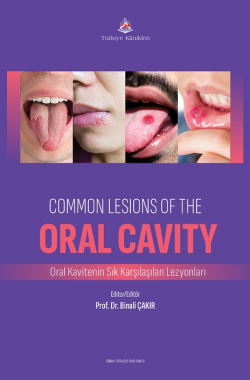
Ceren F, Köse TE. Tongue Disease. In: Çakır B editor. Common Lesions of the Oral Cavity. 1st ed. Ankara: Türkiye Klinikleri; 2025. p.77-95.
ABSTRACT
The development of the tongue begins in the 4th intrauterine week, originating from the mesoderm and ectoderm layers, forming a medial triangular elevation called the median lingual swelling. Immediately after the occurrence of this event, lateral lingual swellings begin to develop on either side of the median lingual swelling. The growing lateral swellings surpass the median lingual swelling and fuse, forming the anterior two-thirds of the tongue. The anterior part of the tongue is formed by the first branchial arch, while the posterior part is formed by the third branchial arch. In muscle development, the second, third, and fourth branchial arches contribute.
Innervation is as follows: the general sensation of the anterior two-thirds of the tongue is innervated by the fifth cranial nerve, while the posterior third is innervated by the ninth cranial nerve. The sense of taste in the anterior two-thirds is innervated by the chorda tympani branch of the seventh cranial nerve, while the posterior part is innervated by both the ninth and tenth cranial nerves.
During the embryological process, the tongue differentiates and becomes specialized, functioning as a mobile organ located at the base of the oral cavity, containing foliate, circumvallate, filiform, and fungiform papillae.
In a healthy state, the tongue is pink in color, and its surface is rough. Any color change or papillary at- rophy on the dorsum of the tongue can be interpreted as a sign of either the onset of a localized disease or a systemic change. The tongue has dense muscle tissue, which plays a crucial role in vital functions such as swallowing and chewing. Also it has functions at speech and taste.
The oral cavity, where the tongue resides, is an area with a high turnover rate, and reactive processes such as neoplasms and lymphatic lesions in this area often affect the surrounding tongue tissue. Many tongue diseases are benign, and identifying and diagnosing benign lesions in the mouth can prevent unnecessary tests for the patient. The lesions we will describe in this section are among the more com- monly encountered lesions in clinical practice, though tongue diseases are not limited to these. It is im- portant to keep in mind that, as part of the body, the tongue can also be affected by pathophysiological events occurring in other regions of the body, leading to changes in its appearance.
Keywords: Tongue diseases; Leukoplakia oral; Glossitis; Macroglossia; Lichen planus
Kaynak Göster
Referanslar
- Thompson DF, Kessler TL. Drug-induced black hairy tongue. Pharmacotherapy. 2010; 30(6):585-93. [Crossref] [PubMed]
- Schlager E, St Claire C, Ashack K, Khachemoune A. Black Hairy Tongue: Predisposing Factors, Diagnosis, and Treatment. Am J Clin Dermatol. 2017;18(4):563-569. [Crossref] [PubMed]
- Gurvits GE, Tan A. Black hairy tongue syndrome. World J Gastroenterol. 2014;20(31):10845-50. [Crossref] [PubMed] [PMC]
- Sawan D, Mashlah AM, Hajeer MY, Aljoujou AA. Assessment of the Possible Correlation between the Presence of Helicobacter Pylori Infection and Hairy Tongue Lesion in a Group of Patients in Syria: A CrossSectional and Pilot Study. Int J Environ Res Public Health. 2023;20(2):1324. [Crossref] [PubMed] [PMC]
- Mohammed F, Fairozekhan AT. Oral Leukoplakia. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
- Mangold AR, Torgerson RR, Rogers RS 3rd. Diseases of the tongue. Clin Dermatol. 2016;34(4):458-69. [Crossref] [PubMed]
- Staines K, Rogers H. Oral leukoplakia and proliferative verrucous leukoplakia: a review for dental practitioners. Br Dent J. 2017;223(9):655-661. [Crossref] [PubMed]
- Kumari P, Debta P, Dixit A. Oral Potentially Malignant Disorders: Etiology, Pathogenesis, and Transformation Into Oral Cancer. Front Pharmacol. 2022;13:825266. [Crossref] [PubMed] [PMC]
- Batsakis JG, Suarez P, el-Naggar AK. Proliferative verrucous leukoplakia and its related lesions. Oral Oncol. 1999;35(4):354-9. [Crossref] [PubMed]
- Van der Waal I., Schepman KP, Van der Meij EH, Smeele,LE. Oral leukoplakia: a clinicopathological review. Oral oncology. 1997;33(5), 291-301. [Crossref] [PubMed]
- Masthan KM, Babu NA, Sankari SL, Priyadharsini C. Leukoplakia: A short review on malignant potential. J Pharm Bioallied Sci. 2015;7(Suppl 1):S165-6. [Crossref] [PubMed] [PMC]
- Parashar P. Proliferative verrucous leukoplakia: an elusive disorder. J Evid Based Dent Pract. 2014;14 Suppl:147-53.e1. [Crossref] [PubMed]
- Gürel G, Şahin S, Aytekin B, Çölgecen E. Oral hairy leukoplakia in the buccal mucosa of a healthy, HIV-negative patient. J Surg Med. September 2018;2(3):339-341. [Crossref]
- Alagöz, Elifhan Atlıhan. Oral Mukozada Görülen Beyaz Lezyonlar. 1. Baskı. Sağlık & Bilim 2022: Odontoloji-Iı.; 2022. [Link]
- Demirkesen, C. Oral Mukoza Lezyonlarında Histopatolojik Yaklaşım. Turkderm-Turk Arch Dermatol Venereol. 2012;46:133-139. [Link]
- Bermejo-Fenoll A, López-Jornet P, Camacho-Alonso F, Saura-Ingles A, Panchon-Ruiz A. Morphometric analysis of the dorsum linguae in patients with Oral Lichen Planus. Med Oral Patol Oral Cir Bucal. 2009;14(8):e388-92.
- Fernández-González F, Vázquez-Álvarez R, Reboiras-López D, Gándara-Vila P, García-García A, Gándara-Rey JM. Histopathological findings in oral lichen planus and their correlation with the clinical manifestations. Med Oral Patol Oral Cir Bucal. 2011;16(5):e641-6. [Crossref] [PubMed]
- Wagner G, Rose C, Sachse MM. Clinical variants of lichen planus. J Dtsch Dermatol Ges. 2013;11(4):309-19. [Crossref] [PubMed]
- Gutiérrez-Venegas G, Sánchez-Carballido MA, Delmas Suárez C, Gómez-Mora JA, Bonneau N. Effects of flavonoids on tongue squamous cell carcinoma. Cell Biol Int. 2020;44(3):686-720. [Crossref] [PubMed]
- Gonzalez M, Riera March A. Tongue Cancer. [Updated 2023 May 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
- Joshi S, Bagade S, Naik C, Deore P, Garad A. Accuracy of Magnetic Resonance Imaging in Detecting Tumor Depth of Invasion in Squamous Cell Carcinoma of the Tongue: A Systematic Review. J Maxillofac Oral Surg. 2023;22(3):720-727. [Crossref] [PubMed] [PMC]
- Ong W, Zhao R, Lui B, Tan W, Ebrahimi A, Clark JR, Soo KC, Tan NC, Tan HK, Iyer NG. Prognostic significance of lymph node density in squamous cell carcinoma of the tongue. Head Neck. 2016;38 Suppl 1:E859-66. [Crossref] [PubMed] [PMC]
- Surej KL, Kurien NM, Sivan MP. Isolated congenital bifid tongue. Natl J Maxillofac Surg. 2010;1(2):187-9. [Crossref] [PubMed] [PMC]
- Siddiqua A, Abubaker P, Saraswati FK, Thakur N. Bifid tongue: differential diagnosis and a case report. Journal of Oral and Maxillofacial Surgery, Medicine, and Pathology. 2015;27: 686-689. [Crossref]
- Emmanouil-Nikoloussi EN, Kerameos-Foroglou C. Developmental malformations of human tongue and associated syndromes (review). Bull Group Int Rech Sci Stomatol Odontol. 1992 Mar-Jun;35(1-2):5-12. [Link]
- James AW, Culver K, Hall B, Golabi M. Bifid tongue: a rare feature associated with infants of diabetic mother syndrome. Am J Med Genet A. 2007;143A(17):2035-9. [Crossref] [PubMed]
- Fleming PS, Flood TR. Bifid tongue - a complication of tongue piercing. Br Dent J. 2005;198(5):265-6. [Crossref] [PubMed]
- Tomara E, Dagla M, Antoniou E, Iatrakis G. Ankyloglossia as a Barrier to Breastfeeding: A Literature Review. Children (Basel). 2023;10(12):1902. [Crossref] [PubMed] [PMC]
- Frezza A, Ezeddine F, Zuccon A, Gracco A, Bruno G, De Stefani A. Treatment of Ankyloglossia: A Review. Children (Basel). 2023;10(11):1808. [Crossref] [PubMed] [PMC]
- Becker S, Brizuela M, Mendez MD. Ankyloglossia (TongueTie) [Updated 2023 Jun 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: [Link]
- Jones H, Hintze J, Walsh M, O'Leary M, Heffernan C. Lingual frenotomy for ankyloglossia in infants with breastfeeding difficulties: a longitudinal observational study. Eur J Pediatr. 2024;183(12):5245-5254. [Crossref] [PubMed]
- Kutti Sridharan G, Rokkam VR. Macroglossia. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
- Topouzelis N, Iliopoulos C, Kolokitha OE. Macroglossia. Int Dent J. 2011;61(2):63-9. [Crossref] [PubMed] [PMC]
- Alarfaj AA, AlHayek AR, Alghanim R, Al-Jazan NA. Self-Induced Traumatic Macroglossia: Case Report and Literature Review. Case Rep Otolaryngol. 2019;2019:6040354. [Crossref] [PubMed] [PMC]
- Thorp MA, de Waal PJ, Prescott CA. Extreme microglossia. Int J Pediatr Otorhinolaryngol. 2003;67(5):473-7. [Crossref] [PubMed]
- Nepram SS, Jain P, Huidrom, RD. Isolated microglossia: A case report. Journal of Medical Society 29(3):p 180-181. [Crossref]
- Voigt S, Park A, Scott A, Vecchiotti MA. Microglossia in a newborn: a case report and review of the literature. Arch Otolaryngol Head Neck Surg. 2012;138(8):759-61. [Crossref] [PubMed]
- Varal IG, Dogan P. Hanhart syndrome: hypoglossia-hypodactylia syndrome. Pan Afr Med J. 2019;32:213. [Crossref] [PubMed] [PMC]
- Lyssy LA, Puckett Y. Oral Hemangiomas. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: [Link]
- Kharkate S, Mohod S, Kukde MM, Tiwari AV, Bute SA. Hemangioma of the Tongue: A Case Report. Cureus. 2024;16(8):e67044. [Crossref] [PubMed] [PMC]
- Sonar PR, Panchbhai A, Dhole P. Tongue Hemangioma on Dorsal Surface: A Case Report. Cureus. 2023;15(11):e48669. [Crossref] [PubMed]
- Gianfranco G, Eloisa F, Vito C, Raffaele G, Gianluca T, Umberto R. Color-Doppler ultrasound in the diagnosis of oral vascular anomalies. N Am J Med Sci. 2014;6(1):1-5. [Crossref] [PubMed] [PMC]
- Jamali Z, Katebi K, Alibabaei H, Jamei Khosroshahi A. Evaluation of the Relationship between Sublingual Varices and Hypertension. Front Dent. 2024;21:7. [Crossref] [PubMed] [PMC]
- Dos Santos Barbosa AC, Palma DIR, Melo MKSS, Costa AKLS, de França GM. Cross-sectional study of sublingual varicosities: systemic exposures. Oral Maxillofac Surg. 2024;28(2):761-766. [Crossref] [PubMed]
- Jafari A, Alaee A, Rezai M, Masoudi M. Evaluation of Sublingual Varices Prevalence and Its Respective Factors in Two Iranian Nursing Homes in 2019. Iran J Otorhinolaryngol. 2022;34(123):165-169. [Link]
- Akkaya N, Ölmez D, Özkan G. Evaluation of the factors associated with sublingual varices: a descriptive clinical study. Folia Morphol (Warsz). 2019;78(2):325-330. [Crossref] [PubMed]
- Srivanitchapoom C, Yata K. Lingual Abscess: Predisposing Factors, Pathophysiology, Clinical Manifestations, Diagnosis, and Management. Int J Otolaryngol. 2018;2018:4504270. [Crossref] [PubMed] [PMC]
- Schweigert J, Christian R, Kemp WL. Challenges in the Diagnosis of a Posterior Lingual Abscess, a Potential Lethal Disorder: A Case Report and Review of the Literature. Am J Forensic Med Pathol. 2020;41(1):64-66. [Crossref] [PubMed]
- Boon M, Pribitkin E, Spiegel J, Nazarian L, Herbison GJ. Lingual abscess from a grill cleaning brush bristle. Laryngoscope. 2009;119(1):79-81. [Crossref] [PubMed]
- Vellin JF, Crestani S, Saroul N, Bivahagumye L, Gabrillargues J, Gilain L. Acute abscess of the base of the tongue: a rare but important emergency. J Emerg Med. 2011;41(5):e107-10. [Crossref] [PubMed]
- Chou J, Walters A, Hage R, Zurada A, Michalak M, Tubbs RS, Loukas M. Thyroglossal duct cysts: anatomy, embryology and treatment. Surg Radiol Anat. 2013;35(10):875-81. [Crossref] [PubMed]
- Amos J, Shermetaro C. Thyroglossal Duct Cyst. [Updated 2023 Jun 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: [Link]
- Gioacchini FM, Alicandri-Ciufelli M, Kaleci S, Magliulo G, Presutti L, Re M. Clinical presentation and treatment outcomes of thyroglossal duct cysts: a systematic review. Int J Oral Maxillofac Surg. 2015 Jan;44(1):119-26. [Crossref] [PubMed]
- Taha A, Enodien B, Frey DM, Taha-Mehlitz S. Thyroglossal Duct Cyst, a Case Report and Literature Review. Diseases. 2022;10(1):7. [Crossref] [PubMed] [PMC]
- Almeida LKY, Silveira HA, Ferrisse TM, Silva EV, Almeida LY, Bufalino A, León JE. Unilateral enlargement of the lateral lingual tonsil: An immunohistochemical study and literature review. Oral Oncol. 2020;109:104857. [Crossref] [PubMed]
- Bower CM. Lingual tonsillectomy, Operative Techniques in Otolaryngology-Head and Neck Surgery. 2005;16(4):238-41. [Crossref]
- Hwang MS, Salapatas AM, Yalamanchali S, Joseph NJ, Friedman M. Factors Associated with Hypertrophy of the Lingual Tonsils. Otolaryngology-Head and Neck Surgery. 2015;152(5):851-855. [Crossref] [PubMed]
- Madani FM, Kuperstein AS. Normal variations of oral anatomy and common oral soft tissue lesions: evaluation and management. Med Clin North Am. 2014;98(6):1281-98. [Crossref] [PubMed]
- Buva K, Deshmukh A, Gupta A, Agrawal S. An intriguing case report of follicular lymphoid hyperplasia of tongue with the detailed review of literature. J Oral Maxillofac Pathol. 2023;27(3):606. [Crossref] [PubMed] [PMC]
- Carnelio S, Rodrigues G. Benign lymphoid hyperplasia of the tongue masquerading as carcinoma: case report and literature review. J Contemp Dent Pract. 2005;6(3):111-9. [Crossref] [PubMed]
- Stoopler ET, Ojeda D, Elmuradi S, Sollecito TP. Lymphoid Hyperplasia of the Tongue. J Emerg Med. 2016 Mar;50(3):e155-6. [Crossref] [PubMed]
- Sands NB, Tewfik M. Benign lymphoid hyperplasia of the tongue base causing upper airway obstruction. Case Rep Otolaryngol. 2011;2011:625185. [Crossref] [PubMed] [PMC]
- Cunha JLS, Roza ALOC, Cruz VMS, Ribeiro JL, Cavalcante IL, Cavalcante RB, Anbinder AL, Abrahão AC, de Andrade BAB, Romañach MJ, Pires FR, Dos Santos-Silva AR, Lopes MA, Vargas PA, Soares CD, de Almeida OP. Oral Lymphoepithelial Cyst: A Collaborative Clinicopathologic Study of 132 Cases from Brazil. Head Neck Pathol. 2022;16(1):268-277. [Crossref] [PubMed] [PMC]
- Wu YH, Kuo YS, Chiang CP, Lin PY. Lymphoepithelial cyst of the tongue. J Dent Sci.2019;14(2):209-210. [Crossref] [PubMed] [PMC]
- Leite BL, Mara Luana B, Severo PT, Oliveira AMC, Medeiros CAG, et al. Lymphoepithelial cyst on the tongue: case report at unusual location. Jornal Brasileiro de Patologia e Medicina Laboratorial, 2017;53(4):273-275. [Crossref]
- Nakayama N, Nakamura S, Sawada K, Iijima Y, Hino S, Kaneko T, Horie N, Lymphoepithelial cyst on the tongue: A case report. Oral and Maxillofacial Surgery Cases. 2023:9(2):1-3 [Crossref]
- Toso A, Colombani F, Averono G, Aluffi P, Pia F. Lingual thyroid causing dysphagia and dyspnoea. Case reports and review of the literature. Acta Otorhinolaryngol Ital. 2009;29(4):213-7. [PMC]
- Nisa L, Morrison S, Levi E. Airway management in patients with lingual thyroid: a case report and review of the literature. Eur Arch Otorhinolaryngol. 2022;279(7):3289-3295. [Crossref] [PubMed]
- Sturniolo G, Violi MA, Galletti B, Baldari S, Campennì A, Vermiglio F, Moleti M. Differentiated thyroid carcinoma in lingual thyroid. Endocrine. 2016;51(1):189-98. [Crossref] [PubMed]
- Sharabi AF, Winters R. Glossitis. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: [Link]
- Chiang CP, Chang JY, Wang YP, Wu YH, Wu YC, Sun A. Atrophic glossitis: Etiology, serum autoantibodies, anemia, hematinic deficiencies, hyperhomocysteinemia, and management. J Formos Med Assoc. 2020;119(4):774-780.https://www.sciencedirect.com/science/article/pii/S0929664619303481?via%3Dihub [Crossref] [PubMed]
- Erriu M, Pili FM, Cadoni S, Garau V. Diagnosis of Lingual Atrophic Conditions: Associations with Local and Systemic Factors. A Descriptive Review. Open Dent J. 2016;10:619-635. [Crossref] [PubMed] [PMC]
- Byrd JA, Bruce AJ, Rogers RS 3rd. Glossitis and other tongue disorders. Dermatol Clin. 2003;21(1):123-34. [Crossref] [PubMed]
- Reamy BV, Derby R, Bunt CW. Common tongue conditions in primary care. Am Fam Physician. 2010;81(5):627-34. [Link]
- Grossman ME, Stevens AW, Cohen PR. Brief report: herpetic geometric glossitis. N Engl J Med. 1993;329(25):1859-60. [Crossref] [PubMed]
- John HA, Ahuja K, Dakhale R, Heda K, Sedani S. Median Rhomboid Glossitis: A Developmental Disorder Involving the Central Part of the Tongue. Cureus. 2023;15(11):e48908. [Crossref] [PubMed]
- Taylor M, Brizuela M, Raja A. Oral Candidiasis. [Updated 2023 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024.
- Ocak H, Er N, Etoz OA, Alkan A. Kıssıng Lesıon-Lookıng Oral Mucosal Irrıtatıon Caused By Smoke Cessatıon Drugs Purchased From A Websıte: Case Report. Ata Diş Hek Fak Derg. 2016;25(3):381-84. [Crossref]
- Shinde SB, Lohe V, Mohod S, Dadgal KV, Priya M, Gurav T. Median Rhomboid Glossitis of the Tongue-Associated Kissing Lesion: A Report of a Rare Case. Cureus. 2024;16(7):e65419. [Crossref] [PubMed]
- Picciani BL, Domingos TA, Teixeira-Souza T, Santos Vde C, Gonzaga HF, Cardoso-Oliveira J, Gripp AC, Dias EP, Carneiro S. Geographic tongue and psoriasis: clinical, histopathological, immunohistochemical and genetic correlation- a literature review. An Bras Dermatol. 2016;91(4):410-21. [Crossref] [PubMed] [PMC]
- Nupur S, Pratik K, Bhavna D, Princy T. Geographic Tongue: A Case Report with Review of Literature. Advances in Human Biology.2016;6(3):p 142-144. [Crossref]
- Chaubal T, Bapat R. Geographic Tongue. Am J Med. 2017;130(12):e533-e534. [Crossref] [PubMed]
- Netto JN, Dias MC, Garcia TR, Amaral SM, Miranda ÁM, Pires FR. Geographic stomatitis: An enigmatic condition with multiple clinical presentations. J Clin Exp Dent. 2019;11(9):e845-e849. [Crossref] [PubMed] [PMC]
- Horiuchi Y. Geographic tongue: What is this disease? J Dtsch Dermatol Ges. 2023;21(12):1465-1467. [Crossref]
- Dafar A, Çevik-Aras H, Robledo-Sierra J, Mattsson U, Jontell M. Factors associated with geographic tongue and fissured tongue. Acta Odontol Scand. 2016;74(3):210-6. [Crossref] [PubMed]
- Feil ND, Filippi A. Frequency of fissured tongue (lingua plicata) as a function of age. Swiss Dent J. 2016;126(10):886-897. English, German. [Crossref] [PubMed]
- Bollen CM, Beikler T. Halitosis: the multidisciplinary approach. Int J Oral Sci. 2012;4(2):55-63. [Crossref] [PubMed] [PMC]
- Danser MM, Gómez SM, Van der Weijden GA. Tongue coating and tongue brushing: a literature review. Int J Dent Hyg. 2003;1(3):151-8. [Crossref] [PubMed]
- Seerangaiyan K, Jüch F, Winkel EG. Tongue coating: its characteristics and role in intra-oral halitosis and general health-a review. J Breath Res. 2018;12(3):034001. [Crossref] [PubMed]
- Nurdiana, Mardina IS. Relationship between glycemic control and coated tongue in type 2 diabetes mellitus patients with xerostomia. Pesquisa Brasileira em Odontopediatria e Clínica Integrada. 2020;19: e5134. [Crossref]